Boost collections
Capture 100% of copays, deductibles, and coinsurance at the time of service.
+$3-6 NRPV
Reduce complexity
Make check-in easy for any staff member with automated processes and a clear next step for every visit.
1 week → 1 hr training
Streamline workflows
Eliminate manual eligibility checks and cost calculations, saving minutes for every patient.
45+ hours per month saved
The easiest way to get insurance right
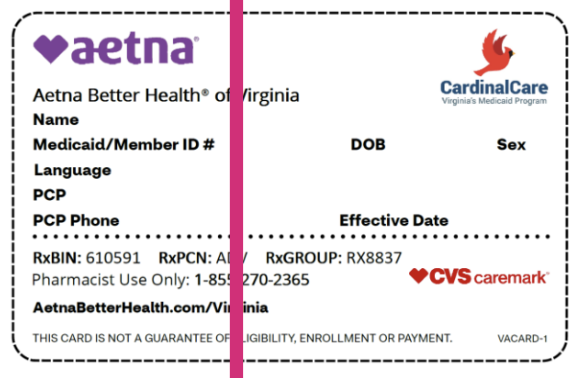
AI OCR
Reads any insurance card and pulls the right info, even edge cases.
AI Insurance Selection
Automatically choose the right payer & plan from thousands, synced to Experity.

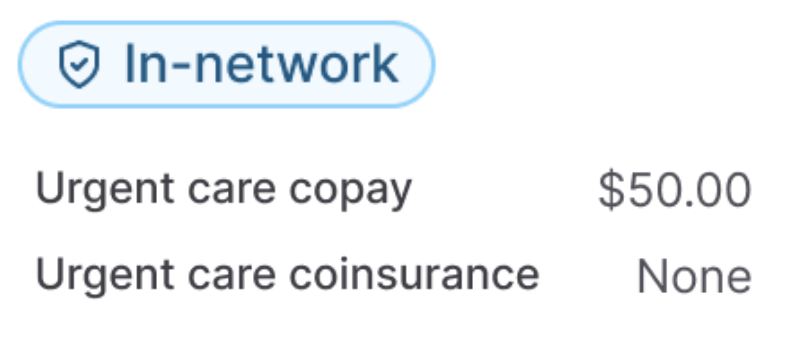
AI Real-Time Eligibility
Instantly confirm in-network status, deductible info, and urgent care benefits.
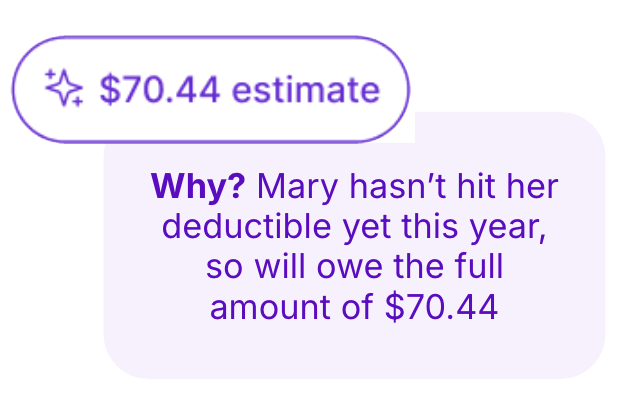
AI Cost Engine
Uses payer contracts and clinic rules to estimate patient cost with a one-line explainer for staff.